Treatment options for urinary incontinence after prostatectomy

Despite improvements in surgical techniques, and robotic assisted prostatectomy in particular, there is still a risk of urinary incontinence following prostate cancer surgery. This type of incontinence is known as Post Prostatectomy Incontinence (PPI).
PPI can affect daily life — from how able you are to work, to how confident you feel in social situations. It can feel embarrassing, stressful to manage, and incredibly isolating.
King Edward VII’s Hospital consultant urologist Mr Jeremy Ockrim takes some time out to discuss how treatment for prostate cancer can lead to urinary incontinence, and what the treatment options are.
What is urinary incontinence?
Urinary incontinence is the involuntary leakage of urine.
In some cases, leakage only occurs in men when they jump, cough, sneeze or laugh. In other cases, leakage can be more severe or continuous, or may occur because they can’t get to the toilet in time.
Stress Urinary Incontinence (SUI) or stress incontinence, is a type of urinary incontinence that happens with physical movement or activity. SUI occurs when control over the external urethral sphincter (the muscle that controls the release or urine from the bladder) is damaged or weakened.
Urge incontinence is when you feel the sudden need to urinate but you don’t always make it to the toilet in time. It can happen as a result of damage to the bladder or nerves that control the bladder.
Either way, it will be a relief to know that urinary incontinence, no matter how severe, can be treated.
How might surgery for prostate cancer cause urinary incontinence?
There are several different treatment options for men with prostate cancer and not all men with prostate cancer need to have surgery.
The main options for men with aggressive prostate cancer are:
- Surgery to remove the prostate, which is called radical prostatectomy
- External radiotherapy
- Internal brachytherapy
- High Intensity Focussed Ultrasound (HIFU).
Each case is different and your specialist doctor will discuss your options with you.
Treatment to remove or destroy the prostate can damage nerves and the external urethral sphincter (which is located right next to the prostate). This then causes stress incontinence.
Damage to the bladder following treatment for prostate cancer can also cause bladder storage problems resulting in urge incontinence symptoms.
How common is urinary incontinence after prostate surgery?
If you have a radical prostatectomy, a tube called a catheter will be placed inside your bladder to allow urine to drain. When the catheter is removed, most men will have some difficulty controlling their urine flow.
For most men, the urinary leakage will improve in the months following surgery. In an NHS trial, 46% of men needed to use absorbent pads six months after having a radical prostatectomy. But, one year on from having the procedure, this figure had improved to 17%.
What are the non-surgical options for treating urinary incontinence?
Pelvic floor exercises (Kegel exercises) have been shown to speed up how quickly the pelvic floor recovers after prostate cancer surgery.
London Urology Specialists have dedicated physiotherapy support for you during this period of recovery, and the British Association of Urological Surgeons has some excellent advice for men on how to perform pelvic floor exercises correctly.
You may also be offered bladder training that can be useful alongside pelvic floor exercises. This involves working with your doctor to learn how to gradually increase the time between needing to urinate and actually urinating. It can take up to six weeks to train your bladder in this way, but it can also be very effective.
Medications may help with overactive bladder symptoms (bladder spasm). Common medications include the antimuscarinics oxybutynin, tolterodine and solifenacin, and the beta-3 agonists mirabegron. These medications work by relaxing the bladder, allowing it to fill with urine and successfully store it without causing urine to leak.
Your doctor will advise what drugs may work best for you and how to take them.
What are the surgical options for treating urinary incontinence?
If your urinary incontinence is severe or isn’t made better by any or a combination of the common non-surgical treatments, your doctor may discuss a surgical treatment with you.
Artificial Urinary Sphincter
For over 40 years, the recognised standard of care for post prostatectomy stress incontinence has been the AMS 800 artificial urinary sphincter. It’s a man-made mechanical device that’s implanted in the body to help control urine leakage for men with severe incontinence.
The device is made up of a cuff, balloon and pump. The cuff is placed around the urethra (water pipe) to prevent leakage. The pump is placed in the scrotum and is pressed to empty the fluid out the cuff, so that you can pass urine. Once urination is finished, the sphincter automatically refills, keeping urine in the bladder and you dry.
The procedure to have the artificial urinary sphincter implanted is carried out while you’re under general anaesthetic. It takes around 90 minutes to perform. The artificial sphincter is implanted through two 5cm incisions: one behind the scrotum and one in the groin crease. These incisions are closed with dissolving stitches. A catheter (bladder tube) is left in place overnight. Most patients are allowed home later that day.
The sphincter is switched off for six weeks to allow tissues to heal. The sphincter is switched on six weeks after surgery during an outpatient visit.
The success rates resulting in complete continence (dry) are 80-90%. The device has a half-life of 10-15 years before a replacement is needed.

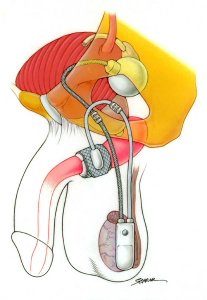
Image source: Boston Scientific
More information about the artificial urinary sphincter can be found in this leaflet from the British Association of Urological Surgeons.
Male Sling
The male sling was first introduced in 2006. The male sling has no mechanical parts and works by supporting underneath the urethra.
The male sling is implanted through a 5cm incision behind the scrotum. The sling is passed through 1cm incisions in the thigh each side, below the urethra. The sling is then tightened to obtain sufficient support. The incisions are closed with dissolving stitches. The surgery takes around 90 minutes.
A catheter (bladder tube) is left in place overnight. This is removed the morning after the surgery. Most patients are allowed home later that day. Your recovery from the surgery will be assessed at your appointment six weeks following surgery.
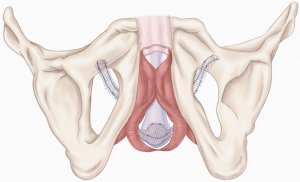
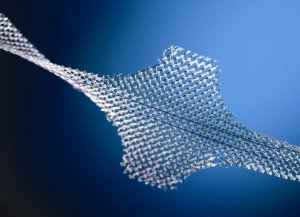
Image source: Boston Scientific
The success rate ranges from 50% to 90%; approximately one third of patients are dry, and one third of patients have substantial improvement depending on how severe their urine leakage was to start.
Male slings are now widely used throughout Europe, America and now the United Kingdom
More information about the male sling can be found in this leaflet from the British Association of Urological Surgeons.
Bulking agent (Bulkamid)
Current standards for treatment are the artificial sphincter or sling implants, but some men consider these too invasive. Because of this, two-thirds of men with incontinence go untreated.
An alternative, a minimally invasive option for men with mild PPI is injection of polyacrylamide hydrogel (Bulkamid). Bulkamid is non-allergenic and stays in the tissues of the body without adverse effects. Success rates between 10 and 30% are expected for patients with mild post prostatectomy incontinence. Injections may be repeated to maintain their effect.
Bulkamid urethral injections are performed as a minimally invasive procedure under day case general anaesthesia. Injections of Bulkamid are performed using a cystoscope (a thin camera). The injections tighten the lining of the urethra.
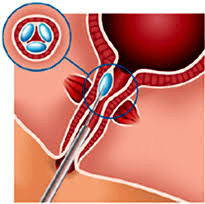
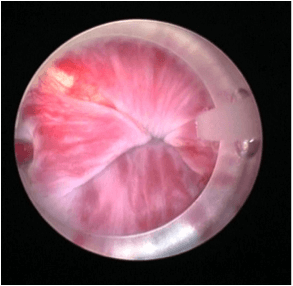
Image source: Research Gate
Image shows view of Bulkamid “cushions” coapting (closing) the urethra.
More information
- If you’re facing prostate cancer surgery or you’ve had it and you’re worried about urinary incontinence, speak to your urologist or cancer specialist. They will be able to discuss your risks and options and if necessary, talk you through treatments for urinary incontinence.
- The Urology Department here at King Edward VII’s Hospital offers treatment and care for prostate cancer and urinary incontinence.
- The KEVII Prostate Cancer Survivorship Centre at King Edward VII’s Hospital can help with post prostatectomy incontinence, erectile dysfunction and all aspects of post-operative recovery, care and support.