What is Diabetic Eye Disease and how is it treated?

King Edward VII’s Hospital Consultant Ophthalmologist, Mr Saruban Pasu is a cataract surgeon and expert in managing diseases of the retina. Part of his role as the clinical lead for the East Sussex Diabetic Eye Screening Programme (DESP) is to ensure all diabetics in the UK receive the highest level of eye care. Here, we…
King Edward VII’s Hospital Consultant Ophthalmologist, Mr Saruban Pasu is a cataract surgeon and expert in managing diseases of the retina. Part of his role as the clinical lead for the East Sussex Diabetic Eye Screening Programme (DESP) is to ensure all diabetics in the UK receive the highest level of eye care.
Here, we speak to Mr Pasu about diabetic eye disease and how it can be prevented and treated.
How does diabetes affect the eyes?
Diabetes is a condition that occurs when your blood sugar levels (also called blood glucose levels) are too high. When we eat a sugary food, or a food containing carbohydrate that’s then broken down into sugars during digestion, our blood glucose levels increase.
Glucose is the favoured source of energy for the body, so we need some sugar in our diet. In someone without diabetes, when blood glucose levels rise, a hormone called insulin is released that then moves sugar from the blood into the muscle cells to be used as immediate energy or stored as glycogen to be used as energy later on.
However, in someone with diabetes, the body either doesn’t make enough insulin to deal with the levels of sugar in the blood, or it cannot effectively use the insulin it does make. This causes long term high blood glucose levels.
These high blood glucose levels can then, over time, cause damage to the nerves, kidneys, other organs and blood vessels. Eventually, the damage to the blood vessels will extend to the tiny blood vessels in the eyes, where they then become blocked or begin to leak. This then causes damage to the retina, leading to diabetic eye disease, or diabetic retinopathy.
The retina is located at the back of the eye and converts the light that enters the eye into electric signals. The brain then receives these signals and interprets them, turning them into the images that you see. The retina relies on oxygen and nutrients delivered to the eye via these tiny blood vessels.
To compensate if these blood vessels become damaged by high blood glucose levels, gradually the eyes begin to grow new blood vessels. But these may not work as well, which can then lead to a loss of vision if diabetic eye disease is not picked up sooner and treated.
Who is at risk of developing diabetic eye disease?
You’re more at risk of developing diabetic retinopathy if you’ve had diabetes for a long time, or it’s particularly poorly controlled.
You may have a higher risk if you also:
- Have high blood pressure
- Are pregnant
- Are of Afro Caribbean or Asian ethnicity
What are the symptoms of diabetic eye disease?
Diabetic eye disease usually develops over several years, and doesn’t normally cause serious problems unless it’s undiagnosed or left untreated. Therefore, you may not notice any symptoms in the early stages.
The condition tends to affect both eyes at the same time, and signs and symptoms to look out for if you have diabetes include:
- Blurred vision
- Floaters – transparent spots or dark strings that float in your field of vision and move in the direction that you’re looking in
- Patches or streaks that block your vision
- Vision that becomes worse at night or in the dark
- A dark spot or empty patch in the centre of your vision
- A sudden and total loss of vision
High blood glucose levels can also lead to the formation of cataracts which can also reduce your level of vision.
Having these symptoms can be frightening and if you’re worried, you should speak to your doctor, optician or ophthalmologist as soon as possible.

Should I have regular eye appointments?
Yes. As a diabetic, you should attend DESP (Diabetic Eye Screening Programme) appointments at least once a year (more regularly if advised to). At these appointments, photographs of your retina at the back of your eye are taken using specialist equipment.
These photographs will be checked for signs of diabetic eye disease and kept as a record of your level of the condition if it’s present to monitor the changes in your eyes over time.
If signs of diabetic eye disease are noted on the photograph, you will be referred to a specialist eye doctor called an ophthalmologist for further discussions about your condition, and treatment if necessary.
You can help to minimise your risk of developing diabetic eye disease by having regular eye health monitoring appointments. You can also help by making sure that you do all you can to keep your diabetes under control, and by taking steps to also control your cholesterol levels and blood pressure.
What are the different stages of diabetic eye disease?
Diabetic eye disease develops over time, in three main stages:
- Stage 1 – background retinopathy – Tiny bulges, called microaneurysms begin to form in the blood vessels at the back of the eye at retina, and these may leak small amounts of blood. This stage doesn’t cause any alteration to your vision, and treatment isn’t usually required, but your condition will be monitored with regular DESP appointments.
- Stage 2 – pre- or non-proliferative retinopathy – At this stage, the small bulges usually cause more widespread leaking of blood, which has a higher risk of affecting your vision.
- Stage 3 – proliferative retinopathy – At this stage, new blood vessels have begun to form, which are weaker and more likely to bleed into the eye, and scar tissue from previous bleeds will begin to form, leading to some loss of vision. There is also a higher risk of you developing a detached retina. If stage 3 diabetic eye disease is left untreated, then you may expect significant sight loss.
During any of these three stages, another condition called diabetic maculopathy can develop. This is a condition that affects the blood vessels of the macular area in the centre of the retina that’s responsible for fine detail vision. Diabetic maculopathy can therefore affect your central vision.
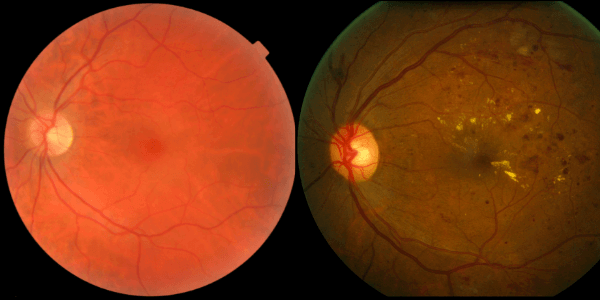
Image Left: Normal eye. Image right: Prolifeative diabetic retinopathy
What treatments are available for diabetic eye disease?
Prevention is the best treatment for diabetic eye disease, and means making sure that your blood glucose levels, cholesterol levels and blood pressure are all well managed. This can be via a healthy lifestyle and/or medications as discussed with your doctor.
Attending your DESP appointments on time will also help to prevent vision loss caused by diabetic retinopathy as the condition can be picked up without you even having symptoms.
Stage 1 and 2 diabetic eye disease isn’t usually treated, and is instead monitored. Stage 3 diabetic eye disease is usually treated with a course of laser treatment to the retina. This slows down the progression of the condition and helps to prevent vision loss.
Intravitreal injections (directly into the clear, jelly like part of the eye called the vitreous humour) of anti-VEGF medications can be as effective as laser treatment for proliferative retinopathy, without the risk of compromising your field of vision. These injections are currently only available as a private treatment and are available here at the King Edward VII’s Hospital.
If laser treatment isn’t successful, then surgery to remove some of the vitreous humour may be necessary. Your doctors will discuss your best course of treatment with you.
More information
- If you have diabetes and you’re concerned about your eye health, speak to your GP or your diabetes specialist medical team. (If you don’t have a GP, you can make an appointment with one of our private GPs.)
- Expert ophthalmology consultants at the King Edward VII’s Hospital Ophthalmology Department specialise in diagnosing and treating diabetic eye disease and other eye complications.
- We also have a specialist Diabetes and Endocrinology Department with leading consultants who can help with all aspects of your diabetes management.
Mr Pasu’s website contains more in depth information and articles on treatments for diabetic eye disease and living a healthy lifestyle to help prevent developing diabetes related eye conditions